Chronic Pain and EDS: Natural Approaches That Really Help

Chronic pain is something that many people live with, yet it’s rarely spoken about in depth. We all understand the sting of a paper cut, the throb of a pulled muscle, or the burn of touching something too hot, but those are short-lived, acute pains. Chronic pain is different. It’s quieter, constant, and often invisible. It changes the way you move, the way you think, and the way you experience life.
For me, pain has been a constant companion. I live with Ehlers-Danlos Syndrome (EDS), a connective tissue disorder that brings with it daily, low-level systemic inflammation. Over the years, I’ve learned that chronic pain isn’t something you “fix”, it’s something you learn to understand, manage, and even work with.
This blog isn’t about miracle cures or quick fixes. It’s about my lived experience: the things I’ve tried, what’s helped, what hasn’t, and the lessons I’ve drawn along the way. My hope is that by sharing my story, I can shine a light for others who are also navigating pain – and perhaps help you start building your own pain relief toolbelt.
Realising My Pain Wasn’t “Normal”
For a long time, I didn’t actually realise that what I was living with was unusual. I grew up in a family where you just got on with things. Injuries, aches, and discomfort were part of life, and I developed a very high pain threshold without even realising it. By the time I was in my teens, I was pushing through dislocated kneecaps on the hockey pitch and carrying on as though it was normal. Pain was simply something I lived alongside.
It wasn’t until I was diagnosed with EDS at 25 that the penny began to drop, what I was experiencing wasn’t what everyone else did. And yet, even then, I didn’t fully grasp the scale of it. I kept going, relying heavily on ibuprofen, which at the time seemed to keep things just about manageable.
By 33, everything came to a head. I found myself facing a serious health crisis: I was given only 6 weeks to live because a parasitic infection had left my bowel at risk of perforation. The years of ibuprofen use may have contributed to the problem, but they weren’t the direct cause. It was a terrifying experience – a stark reminder that relying on painkillers wasn’t a sustainable path.
That moment changed everything. It forced me to step back and look at my body differently. I realised not only that my pain was unique, but that the way I had been coping wasn’t serving me. It was the catalyst for asking deeper questions, exploring natural approaches, and beginning to build a toolbelt of ways to live with and manage chronic pain.
The Emotional Toll and Identity Shift
Getting a diagnosis of EDS was both a relief and a shock. On one hand, it gave me an explanation – finally a name for why my body behaved the way it did. On the other, it was overwhelming to discover that this wasn’t something temporary or curable. It was genetic. It was lifelong. And I was offered little in the way of guidance or support on how to actually live with it.
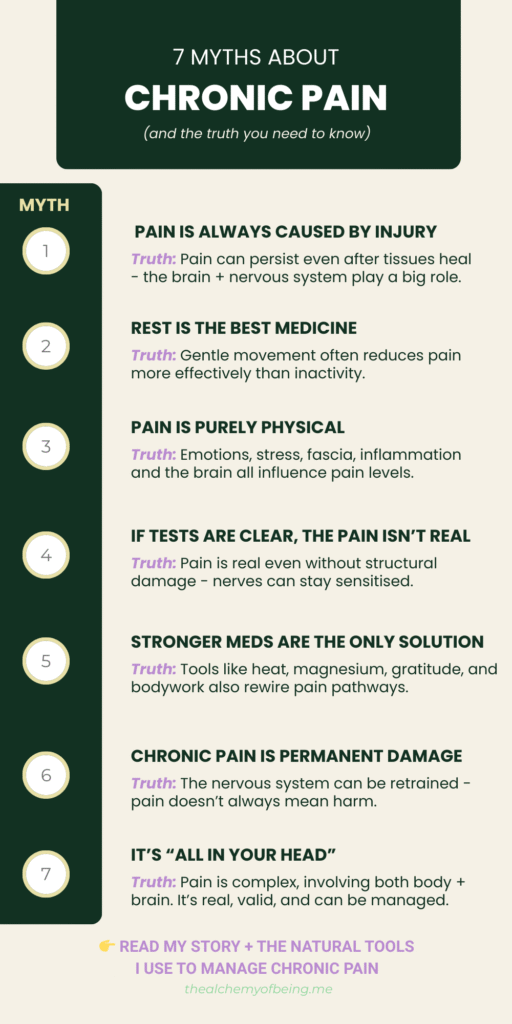
In fact, for years before the diagnosis, I’d been told by doctors that nothing was wrong. That dismissal left a deep mark. When you’re told repeatedly that your pain isn’t real, or that it’s just “in your head,” it chips away at your confidence. It makes you doubt yourself. And when the diagnosis finally comes, it’s not accompanied by a toolkit for survival – just the knowledge that this is how things are going to be.
The advice I was given at the time was crushing in its simplicity: lose weight, and maybe the pain would ease. I was already a healthy, athletic person with strong muscle tone, so the suggestion felt not only unhelpful but insulting. It was as if the medical system had no space for nuance, and certainly no practical tools for someone like me.
Those years taught me something important: I couldn’t rely solely on external answers. If I was going to live well, I needed to learn, to experiment, and to start taking ownership of my own body. That was the beginning of a slow but profound identity shift – from feeling helpless and invalidated to becoming the expert in my own experience.

Living with Chronic Pain Day to Day
For me, living with chronic pain has become less about “pushing through” and more about knowing myself. I’ve learned to pay attention to my body in a way most people never have to. I know my ‘numbers’ – what a good day feels like, what a flare looks like, what recovery requires. That knowledge gives me choice. It means I can still do the things I love, but I plan for them and manage the aftermath.
As a child and teenager, I normalised pain. I threw myself into sport – county tennis and hockey, horse riding – and simply got on with it, injuries and all. Now I approach things differently. I think ahead: Is this activity worth the recovery time? What do I need to do before and after to support my body?
This isn’t defeat; it’s agency. Because I understand my own patterns, I can prepare for a hike, a trip, or a busy week. I know when to dial up or dial-down certain tools, practices and solutions. I know which activities will trigger pain and which will ease it. That knowledge is power. It lets me live a full life within the reality of chronic pain instead of letting pain dictate my life for me.
Understanding the Why
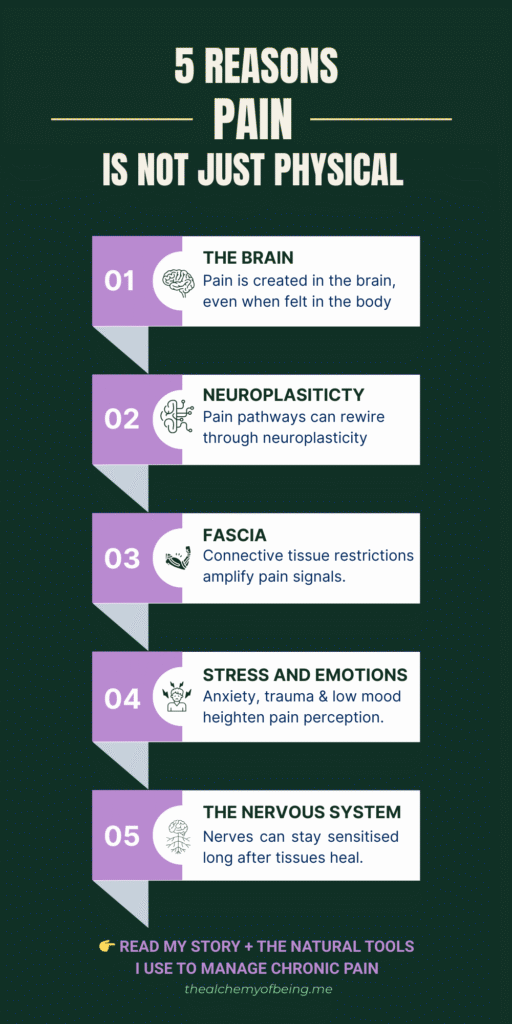
One of the biggest shifts in my journey was realising that pain doesn’t just “happen.” There are reasons. And the more I understood those reasons, the more power I had to do something about them.
For me, two main factors underpin much of my chronic pain: fascia and systemic inflammation.
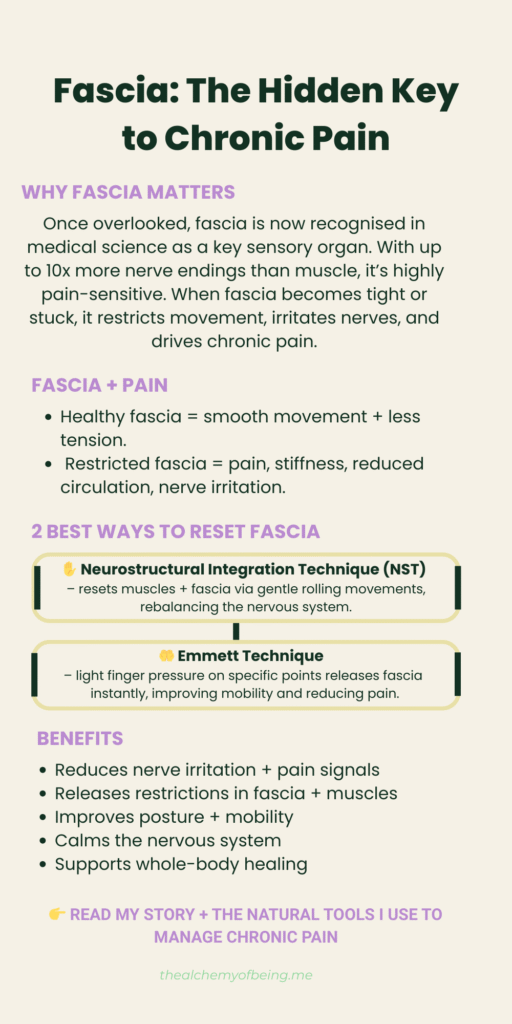
Fascia is a network of connective tissue that wraps around every muscle, organ, and joint in the body. It links everything together – a living web of connection. Because Ehlers-Danlos Syndrome (EDS) is itself a connective tissue disorder, fascia plays a particularly critical role in my experience of pain. When fascia becomes tight, twisted, or restricted, it creates strain patterns that ripple through the body. A restriction in one place can cause pain somewhere completely different.
The fascinating, and frustrating, thing is that fascia has only recently started to be taken seriously in medical science. For decades it was dismissed as unimportant ‘packing material’ that could be cut away without consequence. Now research is showing just how vital fascia is: it’s richly innervated, it influences movement, and it’s deeply involved in pain pathways. For me, discovering fascia’s role was a breakthrough. Therapies like NST (Neurostructural Integration Technique) and Emmett Technique helped me feel the difference immediately – releasing restrictions, easing strain, and softening pain in ways nothing else had managed.
The second piece is systemic inflammation. Low-level, ongoing inflammation doesn’t just make joints ache – it affects the gut, the immune system, energy levels, even mood. Understanding that link was a game-changer. It meant that what I ate, how I managed stress, the supplements I chose, and even my sleep all had a direct impact on how much pain I felt. Reducing that inflammatory load became a cornerstone of my approach.
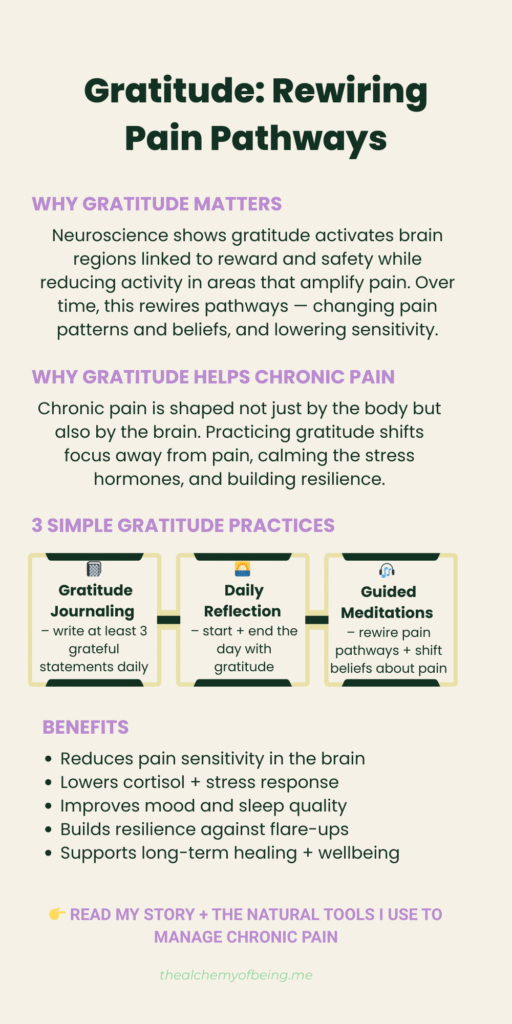
But pain isn’t only physical. What I’ve learned from people like Bruce Lipton and Dr. Joe Dispenza, is that our beliefs and thought patterns also play a role. Stress, negative self-talk, and limiting beliefs amplify pain signals. The brain literally wires those patterns in. On the other hand, meditation, visualisation, and intention can change how the nervous system processes pain. I’ve experienced this myself: a flare that felt unbearable could be softened just by changing my internal dialogue.
When I understood the “why,” everything shifted. Instead of being a passive sufferer, I became an active participant. Pain wasn’t just random or inevitable – it was a message. And if I could interpret the message, I could respond with the right tool from my pain relief toolbelt. Knowledge really is power, and in the context of chronic pain, it’s what gives you back your agency.

Trial and Error: What Didn’t Work
When you live with chronic pain, people are quick to suggest solutions. I’ve tried many of them. Some helped, some didn’t, and a few even made things worse. What I’ve learned is that “failure” isn’t wasted – every attempt teaches you something about your body, your limits, and your needs.
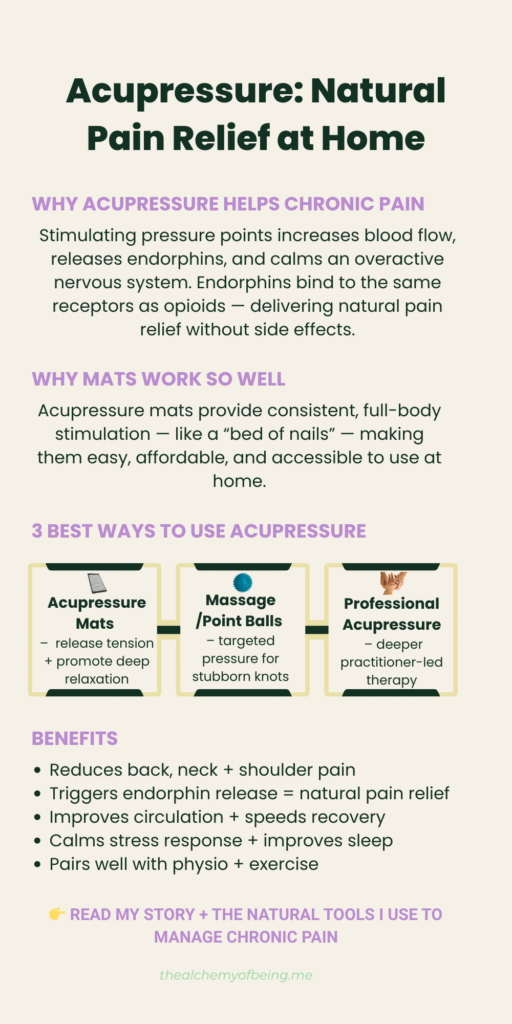
Take acupuncture, for example. For many people it’s life-changing. Acupuncture works by inserting a needle into the body to create a small, controlled inflammation, signalling the body to send healing resources to that spot. For someone with chronic systemic inflammation, like me with EDS, that approach backfired. I didn’t need more inflammation, my body was already on fire. Instead of easing pain, it made it worse. Acupressure, on the other hand, lying on a mat with tiny spikes that stimulate the same points more gently and evenly, has become a daily staple in my toolbelt.
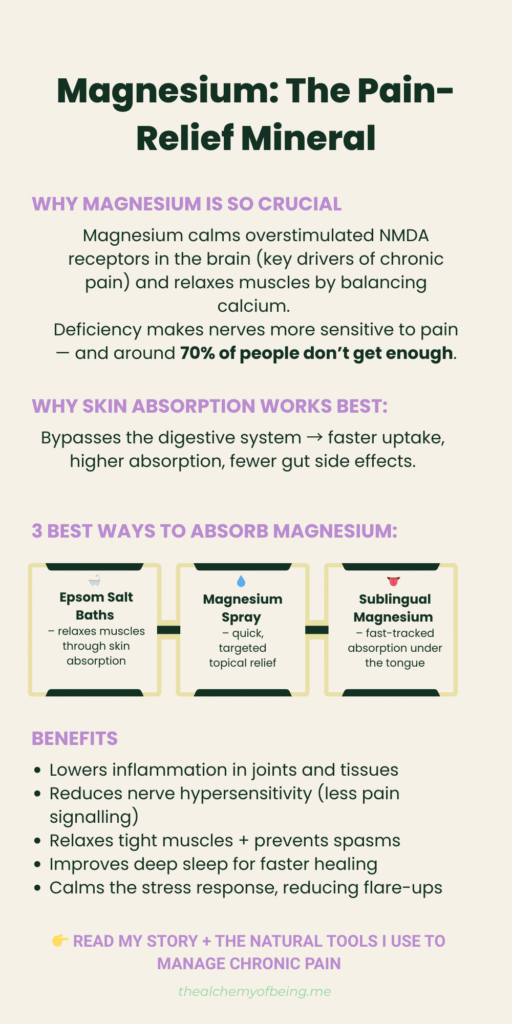
The same pattern showed up with temperature therapies. Cryotherapy and ice-based treatments are praised by some, but I found that extreme cold only increased muscular tension and left me in more pain. What my body responds to instead is heat: hot baths with magnesium salts, far-infrared sauna sessions, or simply wrapping myself in a warm blanket. Where cold created contraction, heat created release.
Those experiences could have left me feeling frustrated, but I chose to see them as part of the process. Knowing what doesn’t work is just as valuable as finding what does. It refines the choices in my toolbelt and makes me more discerning. Pain management isn’t about trying everything – it’s about building the combination that works for you.
Building My Pain Relief Toolbelt: What Helps Me Most
Over the years I’ve built what I call my pain relief toolbelt — and at the centre of it is my morning routine. This isn’t a token wellness ritual; it’s a non-negotiable practice that I’ve refined over years to target inflammation, release tension and give my whole system a neurological reset before the day begins. If I miss it, I feel the difference. When I do it, I start the day grounded, clear and in far less pain.
My Morning Routine
By around 8:45 a.m., before my workday starts, I’ve already completed everything my body needs to manage pain for the day ahead:
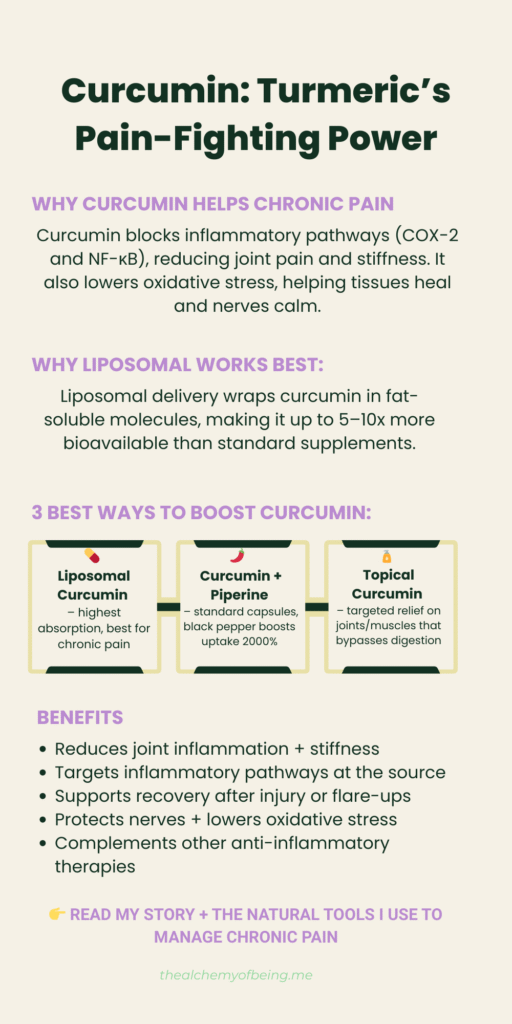
- Hydration & Anti-inflammation: two shots of celery juice, followed by a glass of hydrogen water and a mug of hot lemon water. With this I take my core supplements — liposomal vitamin C, zinc, selenium, MSM and curcumin (turmeric) – to directly support connective tissue, immunity and inflammation pathways.
- Release & Reset: an Epsom salt bath to soothe fascia and muscles, then time on my acupressure mat to stimulate points gently and evenly.
- Neurological Reset: specific sound frequencies designed to change neural patterns rather than just “calm” the nervous system. This helps rewire how my body processes pain.
- Mindset Priming: gratitude and positive affirmations to set my mental and emotional tone for the day.
This whole sequence is my foundation. It’s the reason I can then go into my day with more freedom and less pain.
My Evening Routine
My day doesn’t end without another reset. This is as essential to me as the morning, and just as complete:
- Supplement Support: magnesium, more MSM, and more curcumin.
- Release & Reset: time on my acupressure mat combined with sound frequencies.
- Mindset Downshift: affirmations and gratitude to close the day with calm and focus.
This is its own practice – a deliberate way of starting to release the effects of the day and to signal to my body and mind that it’s time to repair. This means I end the day balanced, supported, and ready for rest.
When Flares Happen
Despite both routines, time and life can cause flare-ups. When they do, I know what to reach for: a more heavily dosed Epsom salt bath, the far-infrared sauna, topical MSM cream, or an extra dose of liposomal curcumin.
Practitioners and Mindset Tools
Alongside my daily rhythms, I also see a NST and Emmett Technique practitioner quarterly for sessions that release fascia restrictions and realign my body. This is like a physical reset that puts everything back to how it should be so that my life doesn’t cause further degradation.
I also regular listen to the podcasts, lectures or interviews with the likes of Bruce Lipton, Dr. Joe Dispenza, Lynne McTaggart, Gary Brecka, Dr Tara Swart and others. Their work underpins my belief that pain isn’t only physical – and that meditation, visualisation, and intention can be just as powerful in shaping how I experience it as supplements or therapies.

Lessons & Wisdom
Looking back, one of the hardest parts of living with chronic pain wasn’t the pain itself – it was the years of being dismissed. I was told repeatedly that nothing was wrong, that my symptoms didn’t add up. And when I finally had a diagnosis, the only advice I was given was to lose weight. For a long time, I placed my trust entirely in the medical model, believing the answers had to come from outside. The more medication I was offered, the worse I felt. It was only when that path failed me that I started to learn the most important lesson of all: I had to become the expert in myself.
Chronic pain has taught me that self-care isn’t indulgence – it’s survival. But it’s not one-size-fits-all. My body responds to some things and not to others, and that’s okay. What matters is discernment: paying attention, experimenting, and keeping what works. That’s resilience, not gritting my teeth and pushing through, but listening to myself and responding with care.
The most surprising discovery has been how much influence I have over my pain. For years I believed relief could only come from doctors, prescriptions, or treatments. Now I know I am my own chemist. My thoughts, beliefs, and choices change how my body experiences pain. That realisation was both shocking and empowering, it gave me back control I didn’t know I had.
If I could offer one piece of advice to someone living with chronic pain – whether you’ve just been diagnosed or you’ve been carrying it silently for years without the support you need – it would be this: don’t hand your power over completely. Doctors and practitioners can play an important role, but they don’t live in your body, you do. It will take time and patience, but you can build your own pain relief toolbelt, unique to your needs, that helps you live more fully. That process won’t erase pain, but it can give you back agency, dignity, and a life you shape on your own terms.
Conclusion and Resources
Living with chronic pain is not easy, but it doesn’t have to mean living without choice. Over time, I’ve learned that pain doesn’t define me. What defines me is how I respond to it, the tools I choose, and the belief that my body holds wisdom if I’m willing to listen.
My story is just one example, but I hope it shows that knowledge really is power. By understanding the “why” behind pain, experimenting with what works and what doesn’t, and curating your own pain relief toolbelt, it is possible to find more freedom, more ease, and more life within the reality of chronic pain.
If you’d like to explore further, you’ll find more therapies and approaches in our Wellness Wiki, a curated list of natural supports we use in our Pain Management Top Picks, and below you can view and download our infographics that highlight practical approaches based on my years of experience.
And remember — don’t find yourself, curate yourself so you can Live your wellness your way.
Please do check out our infographics below:



 Skip to content
Skip to content